Poor or unclear discharge instructions not only have an adverse effect on patient health, but they also have steep consequences for organizations, in terms of increased hospital readmissions. Consider these startling statistics:
- Nearly 20% of all Medicare patients are readmitted to the hospital within 30 days of discharge
- 34% of Medicare patients are readmitted within 90 days of discharge
- As many as 79% of hospital readmissions are considered preventable and result from uncoordinated patient care
Using technology
Discharge instructions communicate important medical information to help patients manage their own care when they leave the hospital. Nonetheless, patients do not always understand these instructions, for a variety of reasons. Non-comprehension of the discharge instructions is associated with decreased compliance and can lead to early hospital readmissions and ultimately, poor health outcomes.
Hospitals have been experimenting with different methods of communicating discharge instructions to improve compliance. For example, Lutheran Medical Center in Wheat Ridge, CO., has seen success from giving discharge instructions to their patients on an Echo recording device. This tool allows healthcare providers to record discharge instructions to patients that they can access from home as frequently as they would like.
Lutheran started with Echo in 2014 in the Surgical and Telemetry Units, both of which have reported high usage of the tool with impressive results:
- 52% decrease in the number of patients with questions or comprehension concerns regarding discharge instructions
- Higher patient compliance and a reduction in nurse callbacks
- Improvement in HCAHPS (Hospital Consumer Assessment of Healthcare Providers and Systems patient satisfaction survey required by CMS for all hospitals in the United States) in areas related to the information that Echo addresses.
According to Lutheran Medical Center administration, they have learned that patients who have had outpatient surgery often can't fully comprehend everything they need to do post-surgery, regardless of how concise and clear their instructions are given.
Through the use of Echo, the instructions are recorded along with any relevant recap of the procedure, and patients then have unlimited access to listen to them. The use of technology has greatly improved the patient experience in other areas, and this tool is a natural evolution of how providers can improve the experience for outpatients as well.
Improving compliance
Discharge instructions are an important part of the discharge process, but patient experience with and use of written instructions has been spotty. The potential roles of discharge instructions to provide security, educate patients, organize medical care and encourage empowerment are lofty and additional work is necessary to ensure provided discharge instructions fulfill this potential.
In an era of increasing pressure to reduce surgical readmissions and with many hospital-based interventions offering limited improvement in readmissions, discharge instructions that connect patients and caregivers to appropriate resources and support patient and caregiver communication with providers following discharge are critical to improving the patient post-discharge experience.
Further resources
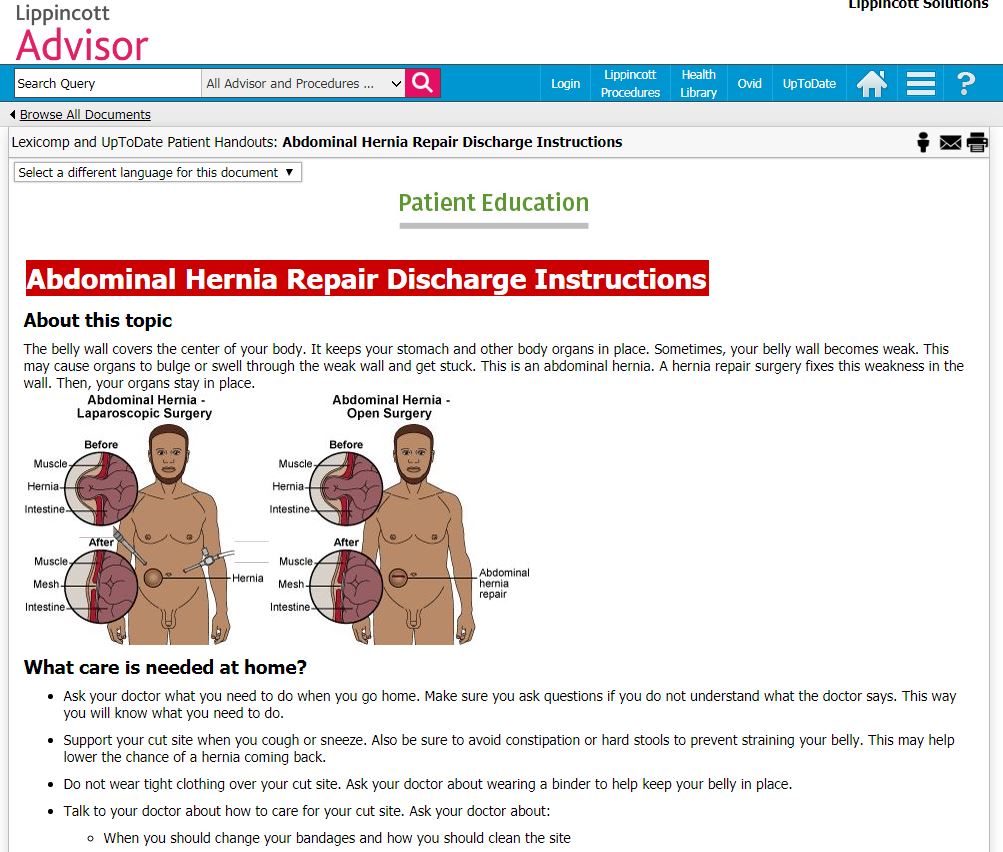
If your organization is struggling with patient discharge compliance and seeing high rates of readmission, let Lippincott® Solutions help. Our leading suite of evidence-based decision support and competency validation software features over 17,000 synthesized content entries and robust patient teaching handouts in Lippincott® Advisor.
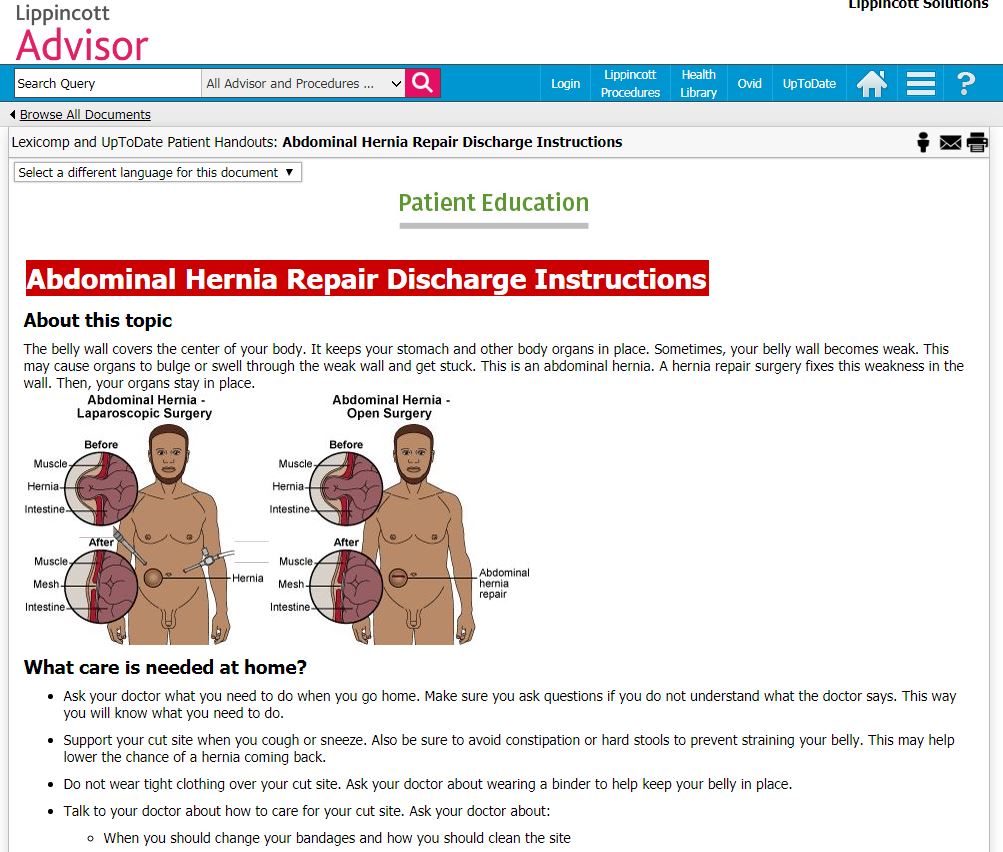
In addition to Lexicomp and UpToDate Patient Handouts and Drug Handouts, Lippincott Advisor also features a Patient Teaching Navigator content set with topics on teaching concepts, learning challenges, as well as diagnostic tests, diseases & conditions and treatments. Click here to learn more.